Patient Ombudsman 2024/25
Learning
Leading
change
Better Experiences
Better Health Care


Patient Ombudsman’s message
“Throughout the year, I speak to many groups about the types of complaints we receive, the resolutions we achieve, and the recommendations we’ve made to address systemic issues through our investigations.”
What Patient Ombudsman does
Patient Ombudsman’s role is to help resolve complaints from patients, long-term care home residents and caregivers about health care experiences in an independent and impartial manner.
2024/25 at a glance
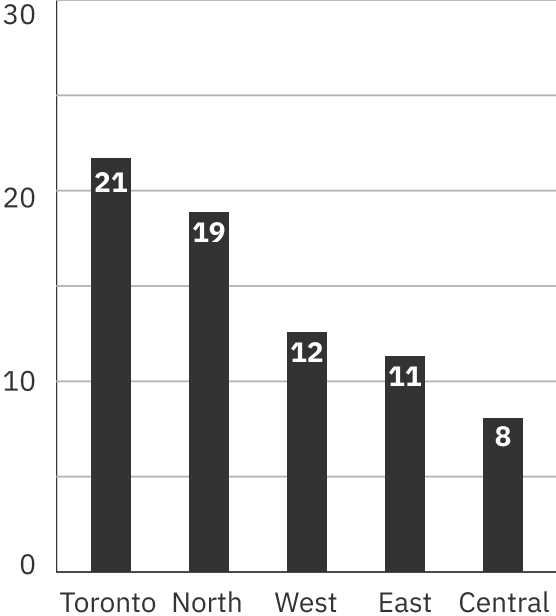
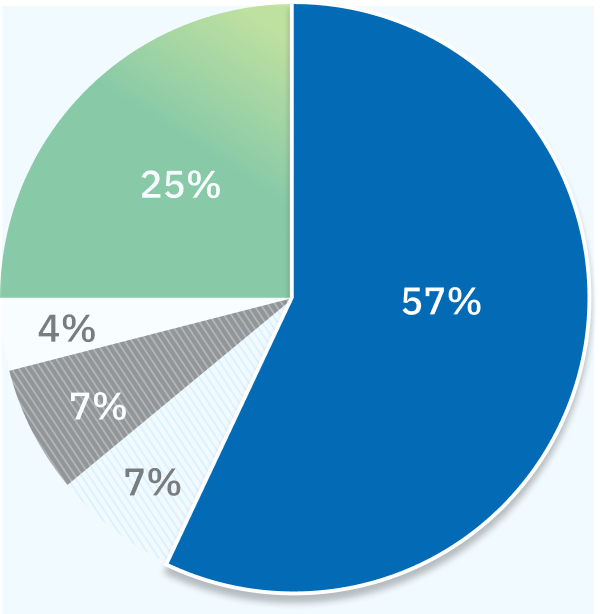
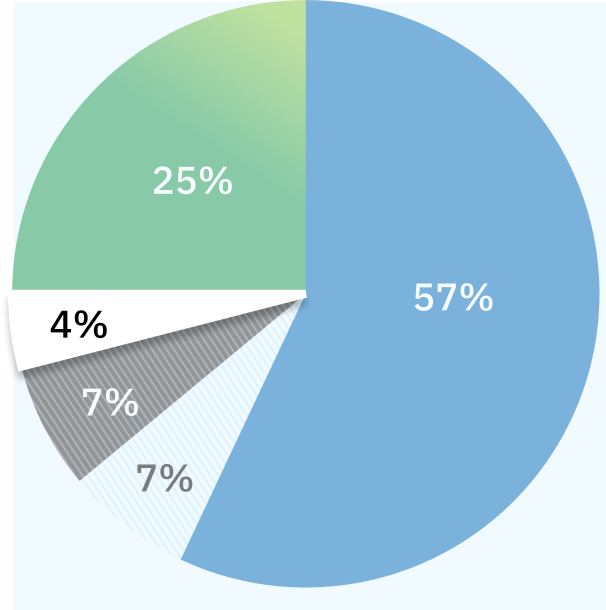
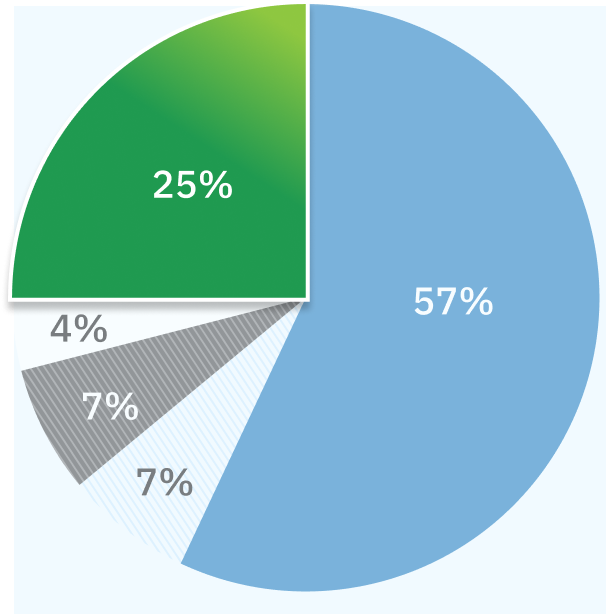
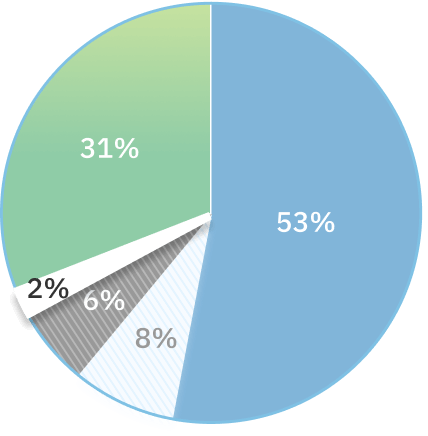
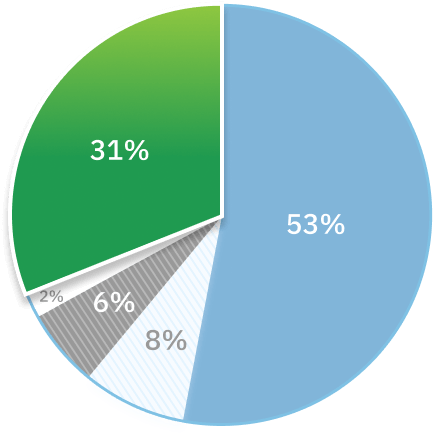
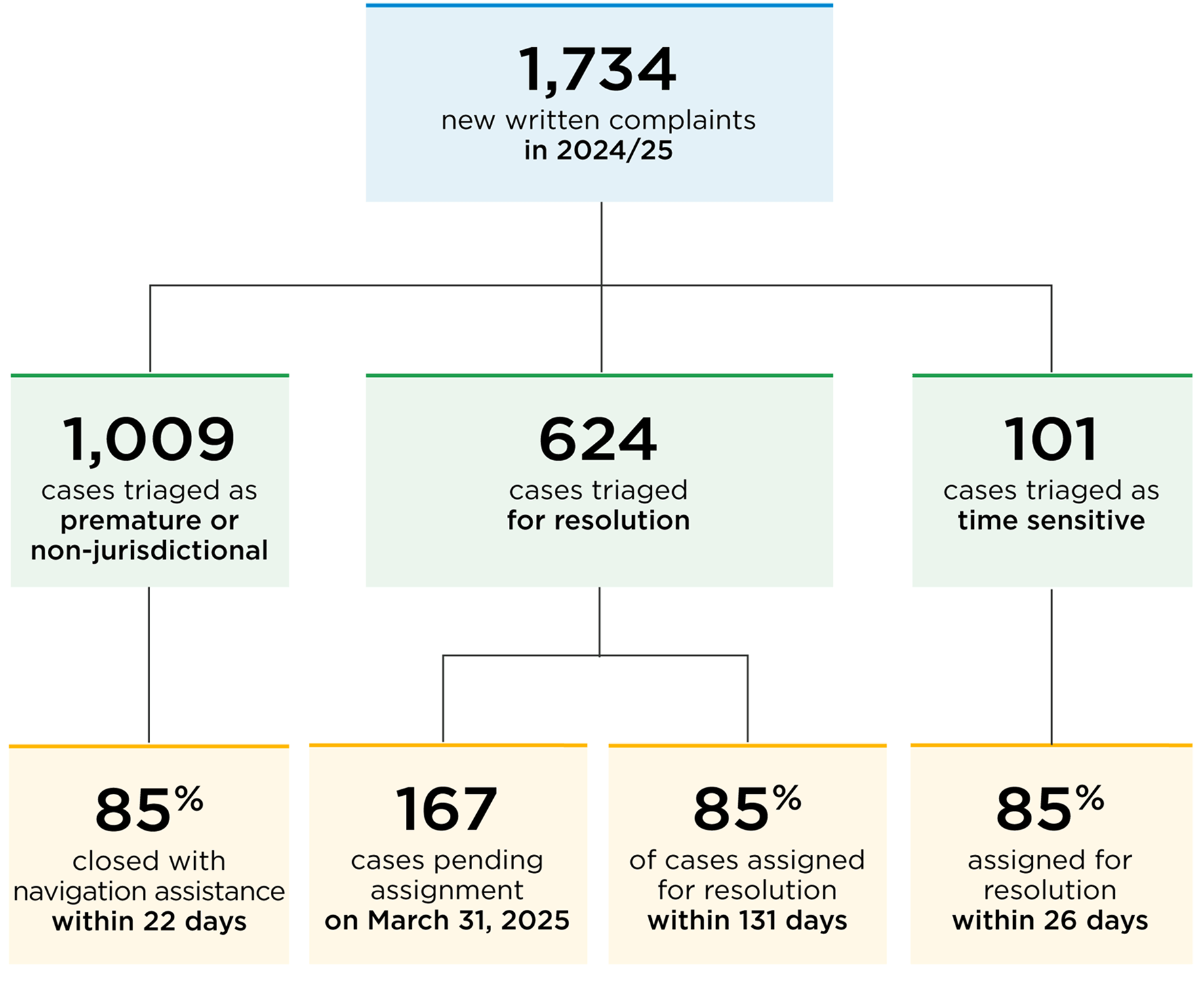
The office received a total of 4,886 new complaints in 2024/25 (April 1, 2024, to March 31, 2025), 1,734 written cases and 3,152 complaints to the call centre. This represents a 16% increase in new written complaints over 2023/24 and an 8% increase in new complaints to the call centre.
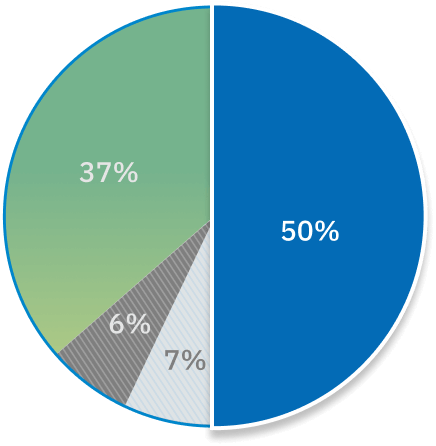
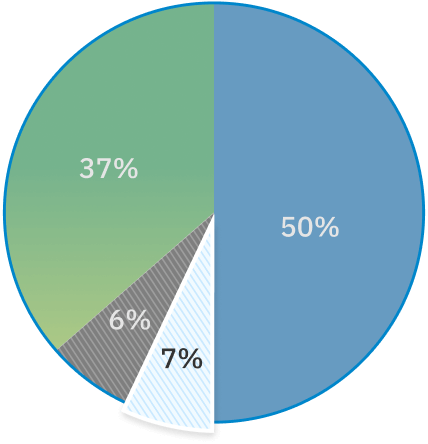
New complaints to Patient Ombudsman by year
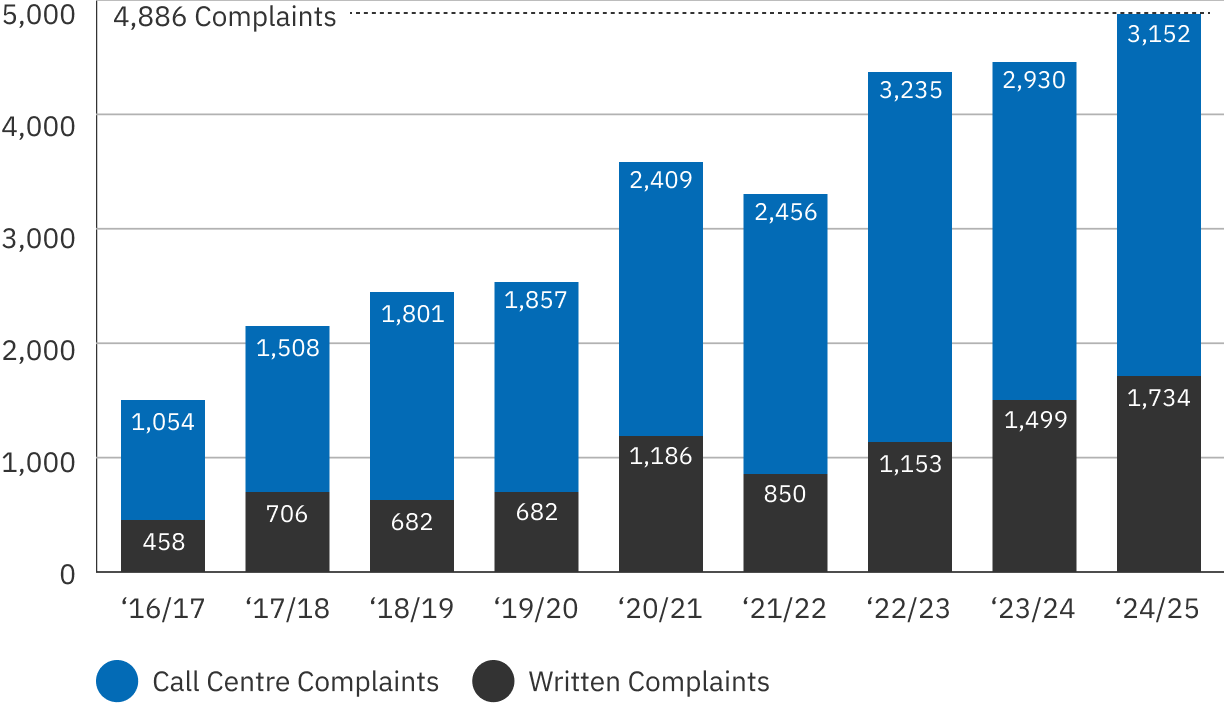
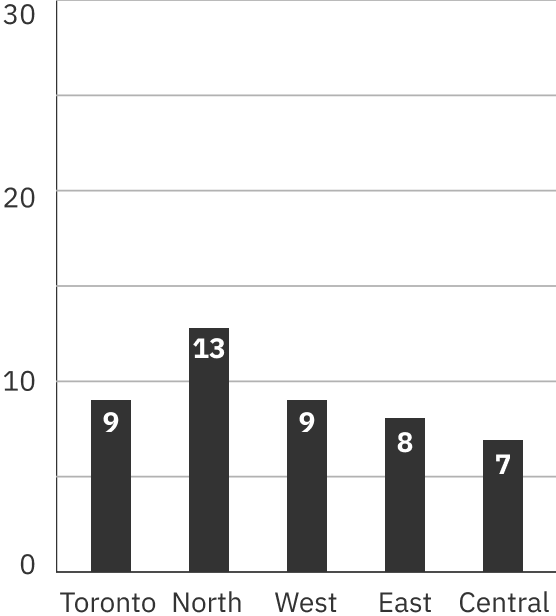
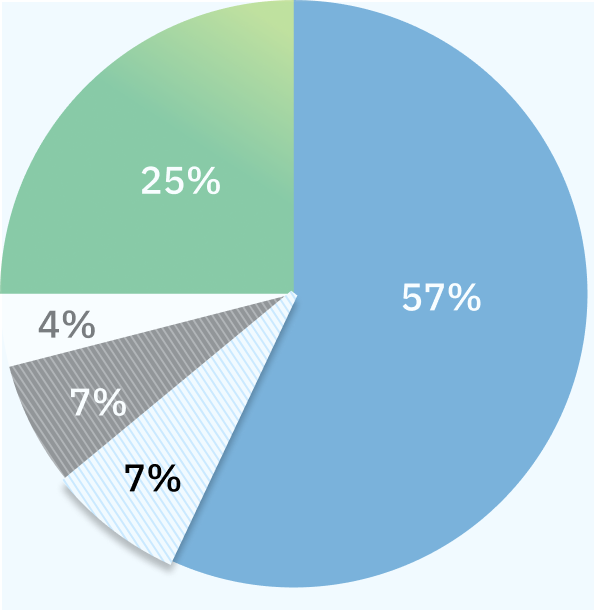
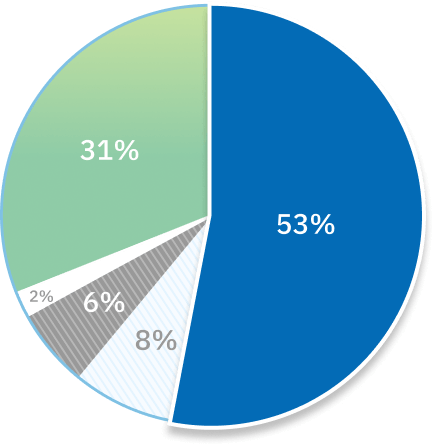
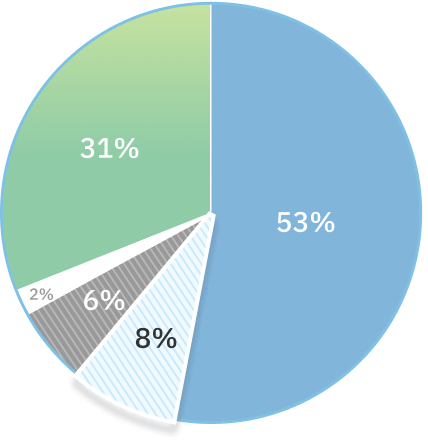
Patient Ombudsman resolved 1,692 written complaints in 2024/25, 4% more cases than 2023/24, but fewer than the number of new cases received. As a result, 306 open cases were carried over into 2025/26.
Patient Ombudsman closed 3,171 complaints to the call centre in 2024/25, an 8% increase over 2023/24. The majority of complaints to the call centre (85%) were resolved within four days, and the exceptions were most frequently because of challenges contacting the complainant to provide new information or respond to complaints left by voicemail.
Spotlight issues
Patient Ombudsman monitors the complaints we receive to identify emerging issues. Our “Spotlight” stories shine a light on the kinds of cases we receive, how we achieve resolutions, and where health sector organizations can look for opportunities to improve patient and caregiver experiences.