Spotlight 1/5
Each year, our annual report presents data on the thousands of complaints that come to our office and how we resolve them on behalf of patients, long-term care residents and caregivers who contact us.
The numbers show what comes in and out of our office; what is harder to show is the work that goes into resolving a complaint.
From the moment someone reaches out to us to the time we consider a case closed, our frontline team is reviewing, evaluating, and helping connect patients and health care organizations.


How we resolve complaints
Whether we make suggestions to health care organizations, or help facilitate an apology, hearing patient, resident and caregiver stories and being able to shine a light on their experiences to ensure better care for others is at the heart of what we do. We also review what steps a health care organization takes to address complaints and ensure that patients, residents and caregivers know how they can give feedback or make a complaint.
When people contact the call centre, Patient Ombudsman’s early resolution staff listen to the person’s concerns and determine if the health care organization(s) is within our jurisdiction and, if so, has the organization had a meaningful opportunity to resolve the person’s concerns directly. It’s important that health care organizations have the chance to respond to complaints directly and have a strong complaint process.1 Given the intimate nature of care, patients and long-term care residents have personal relationships with their health care providers. Having health care organizations respond directly to complaints helps maintain these important relationships.
Complaints in 2024/25
In 2024/25, Patient Ombudsman received 3,152 complaints to the call centre and after discussion with the complainant, 455 were directed to Patient Ombudsman’s online complaint form or were sent a complaint form to assist them in submitting a written complaint. In addition, more than 3,000 complainants were provided with navigation assistance and referrals, including helping 1,467 complainants to connect with patient relations representatives at health care organizations and 1,634 people to connect with other services or oversight bodies.
Patient Ombudsman resolved three-quarters of complaints to the call centre within two calendar days, and 90% were closed within five days. The 10% of cases that were open for five or more days were cases that were re-opened when a complaint called back to provide updates or share additional information, or complaints that required multiple phone calls or emails to re-establish contact. In 246 cases, Patient Ombudsman was unable to contact the complainant after the initial call despite multiple attempts.
As noted earlier in this report, Patient Ombudsman resolved 1,692 written cases in 2024/25 including 142 cases carried over from 2023/24. The resolutions were achieved by:
How do we resolve concerns
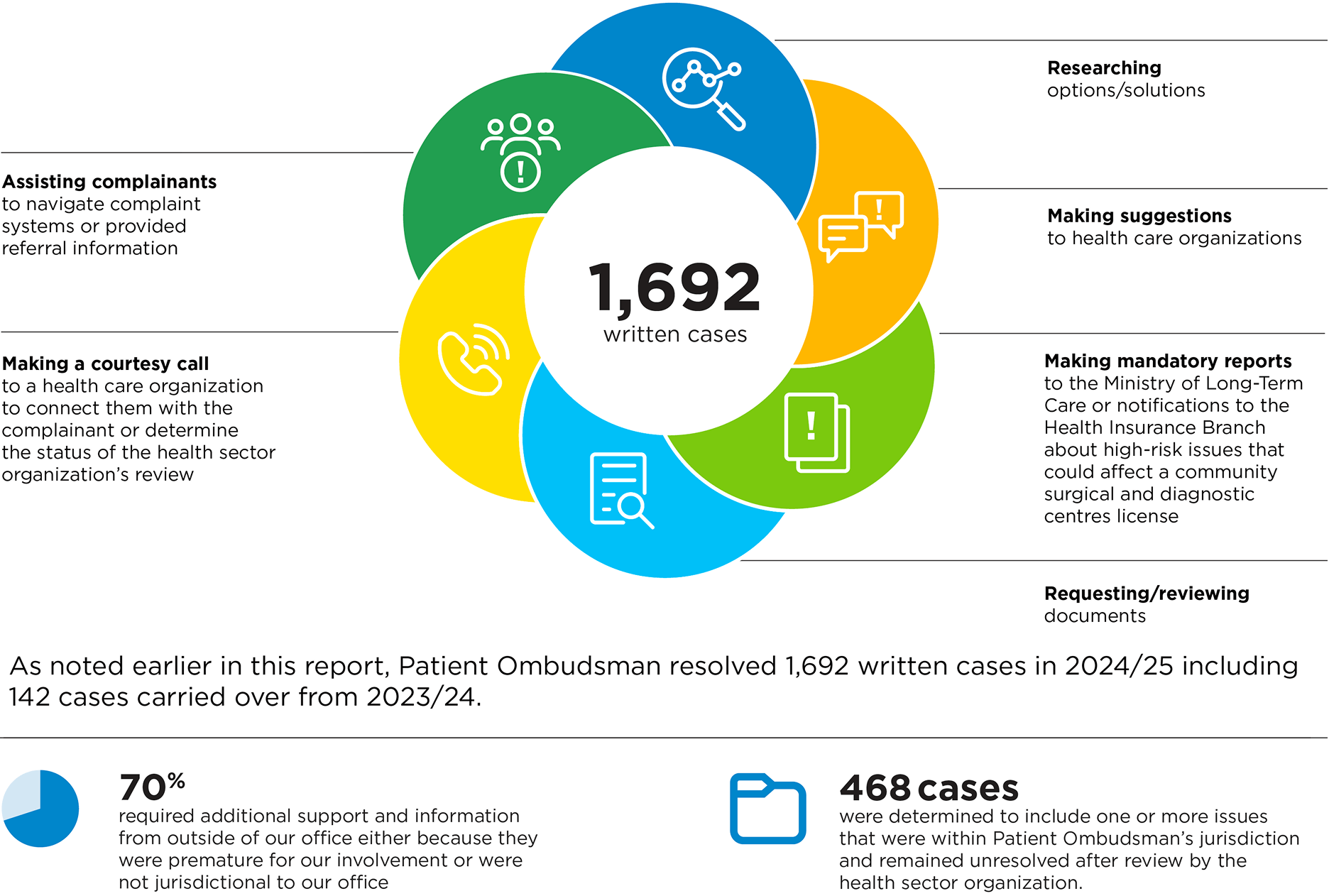
1,692 written cases
Researching options/solutions
Making suggestions to health care organizations
Making mandatory reports to the Ministry of Long-Term Care or notifications to the Health Insurance Branch about high-risk issues that could affect a community surgical and diagnostic centres license
Requesting/reviewing documents
Making a courtesy call to a health care organization to connect them with the complainant or determine the status of the health sector organization’s review
Assisting complainants to navigate complaint systems or provided referral information
As noted earlier in this report, Patient Ombudsman resolved 1,692 written cases in 2024/25 including 142 cases carried over from 2023/24.
70% required additional support and information from outside of our office either because they were premature for our involvement or were not jurisdictional to our office
468 cases were determined to include one or more issues that were within Patient Ombudsman’s jurisdiction and remained unresolved after review by the health sector organization.
Of the 1,692 written cases, 70% required referrals or help connecting with other organizations because the complaint involved issues that were premature for our involvement or were not jurisdictional to our office. Ultimately, 468 cases were determined to include one or more issues that were within Patient Ombudsman’s jurisdiction and remained unresolved after review by the health care organization.
What resolutions look like
Resolutions to written complaints can be as unique as the complaint itself and are guided by the outcome sought by complainants. Some complainants were not seeking a specific resolution but felt it was important to tell their story. Others were seeking an apology, or a change in practice to ensure what happened to them never happens to anyone else. In some cases, complainants are seeking resolutions that Patient Ombudsman cannot assist with, such as financial compensation for a negative experience.
In 133 of the cases that had issues within our jurisdiction, Patient Ombudsman concluded that the health care organization had acted fairly or had responded fairly once they learned of the patient’s concerns. In these cases, Patient Ombudsman often provided information about the health care organization’s actions or response.
Resolution outcomes include the health care organization providing a service, acknowledging or apologizing for what happened, ensuring staff training or education, or updating policies and procedures.
Outcomes achieved
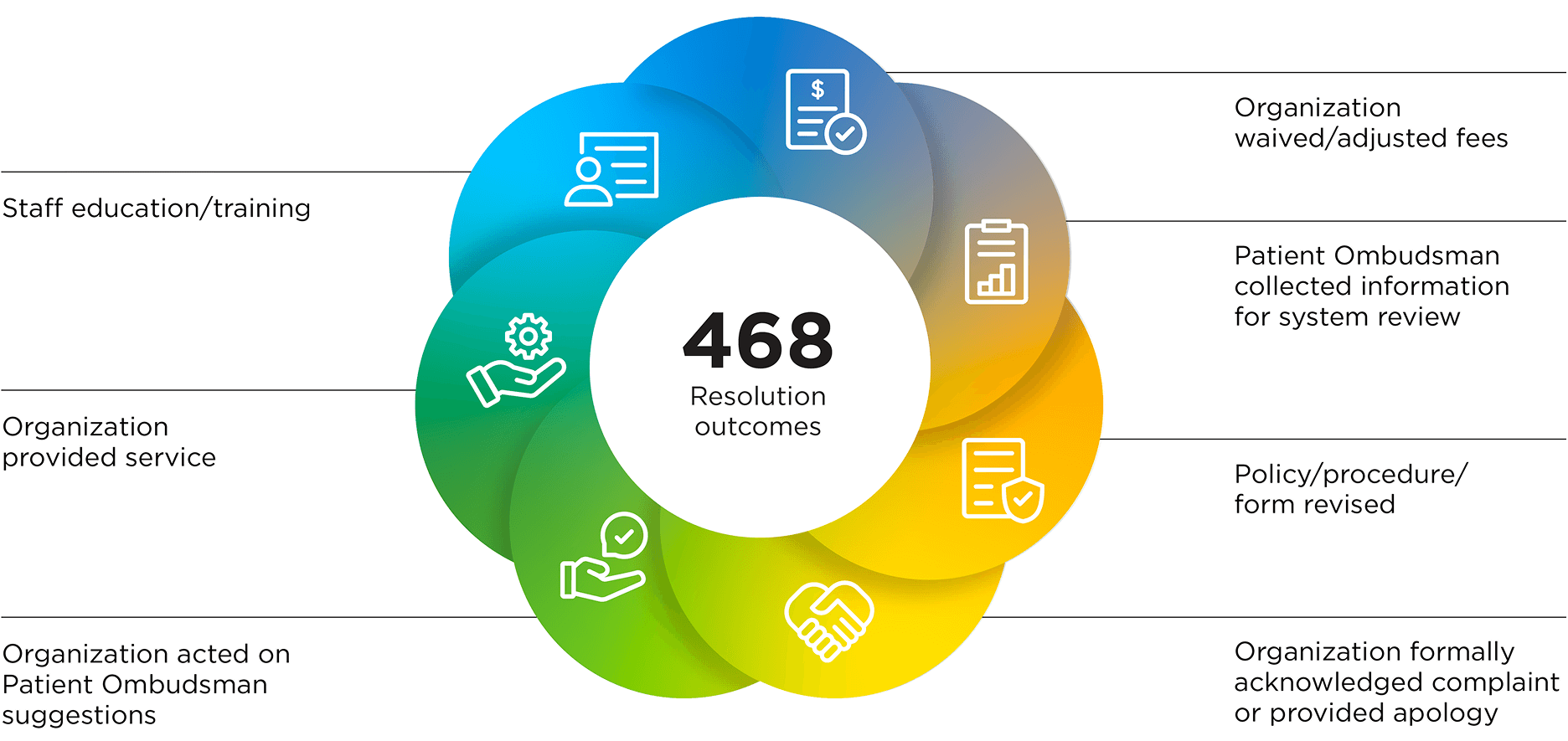
468 Resolution outcomes
Organization waived/adjusted fees
Patient Ombudsman collected information for system review
Policy/procedure/form revised
Organization formally acknowledged complaint or provided apology
Organization acted on Patient Ombudsman suggestions
Organization provided service
Staff education/training
A change in policy can have significant impact because it not only addresses the issue related to the individual complaint, but ensures long-standing change that benefits future patients, residents and caregivers.3 Complaints resolved last year included updates to policies about how health care organizations will address patients’ lost personal property, best practice guidelines for wound care and ensuring complaint policies are patient centred.
